This article aims to answer a common question:
Does BCBS cover drug rehab?
As a leading health insurance provider, Blue Cross Blue Shield (BCBS) offers various plans with different coverage specifics.
We will navigate through the intricacies of BCBS’s policies to provide clear insights into their drug rehab coverage, giving you a comprehensive understanding of BCBS’s role in supporting addiction treatment and recovery journeys.
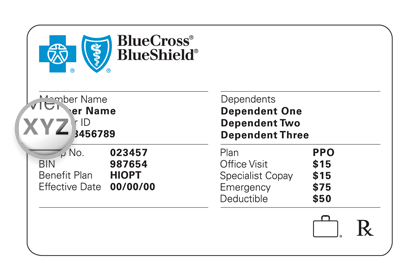
(BCBS Insurance Card Example)
💡 Insurance Advice: Take a proactive approach! Let our Arizona substance abuse treatment center review your Blue Cross Blue Shield (BCBS) insurance benefits for you. Our admissions team can provide detailed insights into the specifics of your policy coverage, guiding you through the financial aspects of accessing treatment. We’re committed to making your journey to treatment as seamless as possible.
Understanding Health Insurance Coverage for Rehab
It is important to understand the coverage provided by health insurance plans for drug rehabilitation, especially for those on the path to recovery.
Companies like BCBS offer such coverage, but the extent of it may vary from one policy to another.
The coverage may include various services – from detoxification and inpatient care to outpatient therapy and follow-up support.
However, it is essential to comprehend the policy details, as they dictate the extent of coverage, the types of services included, and any out-of-pocket costs that might arise.
Knowing your insurance plan – understanding what is covered, the requirements for pre-authorization, and the limits and exceptions – is crucial.
This knowledge gives individuals the power to manage their insurance benefits effectively, ensuring access to necessary treatments while managing financial expectations.
General Components of Drug Rehab
Drug rehabilitation, encompassing various levels of care, is a multifaceted process specifically designed to address the complex nature of addiction and cater to individual recovery needs.
The journey typically begins with detoxification, a medically supervised phase for safely managing withdrawal symptoms.
This initial step is crucial for preparing individuals for subsequent treatments.
Following detox, drug rehab generally involves a combination of residential or inpatient treatment and outpatient programs.
Inpatient treatment offers an immersive environment with 24-hour care, focusing intensively on both psychological and physical aspects of addiction.
In contrast, outpatient treatment allows individuals to maintain their daily responsibilities while attending regular therapy sessions, making it suitable for those with less severe addiction and a stable home environment.
Additionally, drug rehab often includes intermediate options like Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs), which provide a balance between intensive care and the flexibility of outpatient treatment.
Each level, from detox to inpatient and outpatient care, typically incorporates various forms of therapy, such as individual counseling, group therapy, and family therapy sessions.
These therapies are integral in addressing underlying causes of addiction and building coping mechanisms.
Furthermore, rehab programs commonly conclude with aftercare planning and sober living arrangements, essential for relapse prevention and sustaining long-term recovery.
These components, integral to BCBS rehab programs, play a vital role in a holistic approach to addiction treatment, emphasizing physical health, mental well-being, and the journey toward sustainable recovery.
This table provides an overview of the key components of drug rehab, making it easier for individuals to understand the various stages and types of care involved:
| Addiction Treatment Component | Description |
|---|---|
| Detoxification | Medical supervision to manage withdrawal symptoms during the initial detox phase. |
| Inpatient Treatment | Comprehensive care in a residential setting, including medical and psychological support. |
| Outpatient Treatment | Flexible treatment programs that allow individuals to receive therapy while living at home. |
| Individual Counseling | One-on-one sessions focusing on personal triggers and developing coping strategies. |
| Group Therapy | Peer support and shared experiences in a group setting facilitate collective healing. |
| Family Therapy | Engaging family members in the treatment process to mend relationships and build a support system. |
| Medication-Assisted Treatment (MAT) | Combining medication with counseling and behavioral therapies is especially effective for opioid addiction. |
Does BCBS Cover Drug Rehab?
Yes, Blue Cross Blue Shield (BCBS) generally provides coverage for drug rehabilitation, although the extent and details of this coverage may vary significantly based on an individual’s insurance plan.
BCBS recognizes the importance of accessible and effective treatment for substance abuse and addiction, so many of its health insurance policies include rehab coverage.
This coverage usually covers a wide range of treatment modalities, from detoxification services, which are crucial for managing withdrawal symptoms safely, to various rehabilitation programs.
These programs may include inpatient care, where individuals undergo intensive treatment in a residential setting, and outpatient services, which offer flexibility for those who need to maintain their daily routines.
Therapy is also a significant part of addiction treatment, and it is typically included in BCBS coverage.
This therapy often includes individual and group counseling sessions and sometimes family therapy.
BCBS members should review their policy details or directly consult with BCBS to better understand the nuances of their drug rehab coverage, including any limitations, eligibility criteria, and pre-authorization requirements.

Exploring BCBS's Policies on Drug Rehab Coverage
| BCBS Plan Tier | Costs (Premiums & Out-of-Pocket) | Plan Features |
|---|---|---|
| Bronze | Lowest Premiums, Highest Out-of-Pocket Costs | Basic Coverage, Higher Copays/Deductibles, Suitable for Minimal Healthcare Needs |
| Silver | Moderate Premiums, Moderate Out-of-Pocket Costs | Extended Coverage, Moderate Copays/Deductibles, Balanced Coverage and Costs |
| Gold | Higher Premiums, Lower Out-of-Pocket Costs | Comprehensive Coverage, Lower Copays/Deductibles, Ideal for Frequent Healthcare Needs |
| Platinum | Highest Premiums, Lowest Out-of-Pocket Costs | Most Comprehensive Coverage, Minimal Copays/Deductibles, Best for Extensive Healthcare Needs |
Blue Cross Blue Shield (BCBS) offers a variety of health insurance plans, each tiered to cater to different needs and budgets, impacting coverage for services like drug rehab.1
Understanding the differences between these tiers is crucial for selecting the most suitable plan.
• Bronze Plans: These are typically the most affordable in terms of monthly premiums but have higher out-of-pocket costs when accessing care. Bronze plans suit those requiring minimal healthcare services but still want protection against very high costs. Regarding drug rehab coverage, bronze plans may cover basic treatment but could have significant copays or deductibles.
• Silver Plans: Silver plans strike a balance between monthly premiums and out-of-pocket costs. They are a middle-ground option, offering better coverage than bronze plans but with higher monthly premiums. Silver plans may offer more extensive coverage for drug rehab with moderately lower copays and deductibles than bronze plans.
• Gold Plans: These plans typically have higher monthly premiums but lower costs when you need care. Gold plans are advantageous for those who require frequent healthcare services. Gold plans might cover a wider range of treatment options in drug rehab contexts with more favorable cost-sharing terms.
• Platinum Plans: The highest tier, platinum plans, have the highest monthly premiums but the lowest out-of-pocket costs. They are ideal for those who need extensive medical care. For drug rehab, platinum plans likely offer the most comprehensive coverage, including various treatments and therapies, with minimal copays and deductibles.
It’s essential to note that within each plan tier, the specifics of drug rehab coverage can vary based on the state and the individual BCBS plan.
Members should carefully review plan details or consult with BCBS representatives to understand the nuances of rehab coverage, including therapy types, duration of treatment, and any required pre-authorization.
This careful consideration ensures that individuals choose a plan that aligns with their healthcare needs and financial capabilities, providing the necessary support for addiction recovery.
BCBS’s Coverage of Therapies and Treatment Modalities in Drug Rehab
Blue Cross Blue Shield (BCBS) provides coverage for a diverse array of therapies and treatment modalities in the realm of drug rehabilitation, recognizing the multifaceted nature of addiction treatment.
This coverage typically includes traditional therapy forms such as individual counseling, which offers personalized guidance and support, and group therapy, fostering a sense of community and shared recovery.
Many BCBS plans also extend coverage to family therapy, acknowledging the role of family dynamics in addiction and recovery.2
Apart from these, BCBS often covers more specialized treatment modalities like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), both of which are effective in addressing the underlying psychological patterns of addiction.
The inclusivity of these treatments in BCBS plans underscores a comprehensive approach to addiction treatment, aiming to provide members with the necessary tools for a successful and sustained recovery.
However, the coverage for these therapies can vary based on the specific plan, so members are advised to review their policies or consult with BCBS for detailed information.
The goal is always to provide a continuum of care that supports long-term recovery and equips individuals with the skills needed to maintain sobriety post-treatment.
Medications for Drug Addiction Treatment Covered by BCBS
Blue Cross Blue Shield (BCBS) typically extends its coverage to include medications used in the treatment of drug addiction, recognizing their importance in a comprehensive approach to addiction recovery.
This coverage aspect is particularly crucial for Medication-Assisted Treatment (MAT), which combines pharmacological interventions with counseling and behavioral therapies.
MAT is often used in treating opioid use disorders, employing medications like Methadone, Buprenorphine, or Naltrexone to manage withdrawal symptoms and cravings, thereby reducing the likelihood of relapse.3
BCBS plans usually cover these medications, but the extent of coverage can vary depending on the specific policy details and requirements.
Some plans might require pre-authorization or have specific guidelines on the duration and dosage of medication coverage.
By including these medications in their coverage, BCBS enables members to access essential components of addiction treatment, which can significantly enhance the effectiveness of the recovery process.
Policyholders are encouraged to closely review their plans or consult with BCBS representatives to understand the specifics of their coverage for addiction treatment medications.
BCBS’s Approach to Coverage for Drug Addiction and Co-Occurring Disorders
Insurance coverage for drug addiction and co-occurring disorders, particularly in plans offered by providers like Blue Cross Blue Shield (BCBS), is increasingly recognizing the interconnection between substance use disorders and mental health conditions.
These co-occurring disorders, also known as dual diagnoses, often require an integrated treatment approach that addresses both the addiction and the concurrent mental health issues, such as depression, anxiety, or bipolar disorder.
BCBS plans typically cover a range of treatments that include not only the therapies and medications necessary for addiction recovery but also those vital for the treatment of accompanying mental health disorders.
This holistic approach may encompass psychiatric evaluations, medication management for mental health conditions, individual and group psychotherapy, and specialized programs tailored to dual-diagnosis patients.
Coverage specifics can vary based on individual policies, with certain limitations or prerequisites often in place.
However, the trend in healthcare coverage is increasingly towards a more inclusive understanding of addiction treatment, acknowledging the need for comprehensive care that addresses the full spectrum of a patient’s health challenges.
Policyholders dealing with dual diagnoses are advised to thoroughly review their insurance plan or consult with their provider to understand the extent of their coverage for both addiction treatment and mental health care.
Navigating BCBS’s Limitations and Exclusions in Health Insurance for Drug Rehab
Understanding the limitations and exclusions in health insurance policies is a critical aspect of effectively utilizing coverage, especially in the realm of addiction treatment.
Each health insurance plan, including those from providers like Blue Cross Blue Shield (BCBS), comes with its own set of defined boundaries and exceptions which can significantly impact the scope of treatment available to the insured.
These limitations can manifest in various forms, such as restrictions on the length of treatment covered (e.g., a capped number of days for inpatient rehab), exclusions of certain types of therapies or treatments, or limitations on the frequency of therapy sessions.
Additionally, some plans may not cover certain medications or exclude experimental or non-traditional treatments.
Exclusions may also apply to services provided by out-of-network facilities or providers.
It’s essential for policyholders to thoroughly review their insurance documentation or consult with their insurance provider to gain a clear understanding of these limitations and exclusions.
This knowledge helps in planning for any potential out-of-pocket expenses.
It ensures that individuals can make informed decisions about their treatment options, aligning their choices with the coverage available.
Checking Your BCBS Coverage for Rehab
Determining the specifics of your Blue Cross Blue Shield (BCBS) drug rehab coverage is crucial in preparing for addiction treatment.
The most direct way to understand your coverage is by reviewing your policy documents, which provide detailed information about covered services, limitations, and prerequisites such as pre-authorization.
These documents often outline the types of treatments covered, including inpatient and outpatient services, therapy sessions, and medication coverage.
If the policy documents are unclear immediately, contacting BCBS directly through their customer service line can provide clarity.
Customer service representatives can explain the nuances of your coverage, answer specific questions, and guide you through obtaining any necessary pre-authorizations.
Additionally, many BCBS plans offer online portals where members can access their coverage details and find approved providers.
For a more personalized insight, consulting with healthcare providers or addiction treatment specialists who are familiar with BCBS policies can also be beneficial.
They can help interpret coverage in the context of your specific treatment needs and assist in navigating the approval process for rehab services.
Taking these steps to understand your BCBS drug rehab coverage thoroughly ensures that you can access the necessary treatment with a clear understanding of financial responsibilities.
Finding BCBS-Approved Drug Rehab Treatment Centers
Choosing the right treatment center is crucial for effective recovery, and for those insured by Blue Cross Blue Shield (BCBS), selecting a BCBS-approved rehab is essential for ensuring coverage.
BCBS has a network of approved treatment centers that meet their standards for quality and care.
To find BCBS-approved centers, members can use BCBS’s online directories, consult healthcare providers for recommendations, or verify directly with the treatment center.
Choosing an approved center is vital for coverage eligibility, quality assurance, and coordinated care between the treatment center and BCBS.
We Accept BCBS Health Insurance at Cornerstone!
Cornerstone Healing Center in Arizona is proud to be an addiction treatment center that accepts Blue Cross Blue Shield (BCBS) health insurance policies!
Our affiliation with BCBS means that clients with BCBS insurance can access our BCBS drug rehab services with the assurance that their treatment is covered.
At Cornerstone, we offer a range of treatment options tailored to meet individual needs, including inpatient and outpatient programs, therapy sessions, and co-occurring disorders, all within BCBS’s coverage policies.
We understand that navigating insurance coverage can be complex and sometimes overwhelming, so we offer to verify your insurance coverage for free!
Reach out to us today to begin your confidential assessment!