Cornerstone
Aetna Substance Abuse Treatment
Learn about alcohol and drug treatment coverage and get help at our Arizona rehab centers that accept Aetna's policies
Arizona Aetna Drug Treatment
Jump to the following sections
View our addiction treatment locations
Now Accepting AHCCCS Health Choice,
Mercy Care, TriCare, and Triwest
Addictions we treat at Cornerstone
Aetna Covered Drug Rehab Programs

Our Residential Treatment Programs provide comprehensive and continuous support for individuals struggling with substance abuse. We integrate detoxification, counseling, and holistic practices for healing. Our evidence-based therapies include Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), and we incorporate mindfulness, yoga, and art therapy. Our goal is to help individuals address the underlying factors of addiction and equip them with effective tools for long-term recovery and relapse prevention.

Our Partial Hospitalization Programs (PHP) for substance abuse are designed to offer a comprehensive and structured approach to recovery. The program operates five days a week for six hours daily and provides intensive daytime treatment, including therapy, group sessions, and holistic practices, without requiring overnight stays. This approach helps individuals identify and address their addiction while providing them with the necessary skills and support to maintain long-term sobriety. PHP emphasizes accountability and encourages individuals to apply what they have learned in real-world situations.

Our Intensive Outpatient Program (IOP) is the first step in the process, followed by the standard Outpatient Program, which operates three days a week with a flexible schedule to accommodate personal commitments and responsibilities. These Outpatient Programs comprise various therapeutic activities, including individual counseling, group therapy, and workshops for skill development. Our comprehensive approach ensures a supportive pathway to healing and rebuilding lives affected by addiction.
Aetna Health Insurance
Aetna is an insurance company with a reputation for providing healthcare services to individuals and employers. Headquartered in Hartford, Connecticut, Aetna has become a leading health insurance provider nationwide, offering various plans, such as medical, dental, and behavioral health coverage. Aetna is known for its dedication to enhancing access to quality care. It serves millions of members throughout the United States, striving to impact health and well-being positively.1
About Aetna Drug Treatment Coverage
Aetna is dedicated to promoting holistic health and well-being. As part of this commitment, it offers substance abuse treatment coverage to support individuals through every stage of their recovery journey. Aetna’s drug rehab coverage includes detox, inpatient, residential, outpatient, therapy, and counseling services for substance abuse.2 Aetna provides personalized care by collaborating with a network of qualified providers to ensure that members receive the appropriate level of care. The company’s approach is comprehensive, addressing not only the physical aspects of addiction but also the psychological and social factors, thereby supporting a more sustainable recovery.3
Alumni Client Family Testimonial
I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does Aetna Provide Coverage For?
Addictions Covered by Aetna
Aetna policies offer comprehensive coverage for substance abuse disorders, including alcohol and drug rehab. Here are some addictions treated by our Arizona facilities that are likely covered by your Aetna health insurance:
- Alcohol: Holistic programs for alcohol addiction recovery are covered by Aetna insurance.
- Opioids: Aetna provides comprehensive care and support for those overcoming opioid addiction.
- Fentanyl: Treatment for fentanyl addiction, including specialized care and support, is covered by Aetna insurance.
- Cocaine: Aetna covers specialized treatment plans designed to combat cocaine dependency and foster sustained sobriety.
- Methamphetamine: Aetna insurance supports methamphetamine addiction treatment, focusing on core issues for effective recovery.
- Benzodiazepine: Treatment programs aimed at benzodiazepine withdrawal and rehabilitation are covered by Aetna insurance.
- Co-Occurring Disorders: Aetna coverage includes tailored therapy for individuals diagnosed with co-occurring addiction and mental health conditions.
our Arizona treatment programs covered by Aetna
Meet Our Clinical Team

Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.

Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About Using Aetna Benefits to Pay for Substance Abuse Treatment
What types of drug rehab programs does Aetna Health cover?
Aetna, as a prominent insurance provider, typically covers various types of addiction treatment under its health plans, though the exact coverage can vary based on the specific plan, location, and other factors.
Generally, Aetna plans may include coverage for the following types of addiction treatment:
Detoxification: Medically supervised detox is often the first step in treating substance use disorders. It helps manage withdrawal symptoms safely and effectively.
Inpatient Rehabilitation: Residential programs offer specialized care and support 24/7 at a live-in treatment facility, including medical and psychological treatment.
Outpatient Rehabilitation: Outpatient treatment enables individuals to receive services while living at home. Services can involve counseling, therapy, and medical care.
Partial Hospitalization Programs (PHP): PHP offers a middle ground between inpatient and outpatient care. During the day, patients receive intensive treatment, while at night, they can stay at home.
Intensive Outpatient Programs (IOP): IOP provides comprehensive outpatient services by offering a wider range of therapy and related activities.
Medication-Assisted Treatment (MAT): MAT pairs medications like Methadone and Buprenorphine with counseling to treat addiction.
Therapy and Counseling: A range of therapeutic techniques, including Cognitive Behavioral Therapy (CBT) and family therapy, address psychological aspects.
Aftercare Support: Ongoing support after formal treatment, such as 12-step programs, sober living homes, and relapse prevention planning, might also be covered.
Those insured must consult their specific Aetna plans regarding coverage details, costs, in-network stipulations, preauthorizations, and treatment limitations.
Connecting with an Aetna agent or medical provider can also offer guidance tailored to unique needs.
How long will Aetna cover my stay in rehab?
How do I find out what my policy covers?
Follow these steps to obtain accurate information about your Aetna insurance policy coverage, including addiction treatment and other medical services:
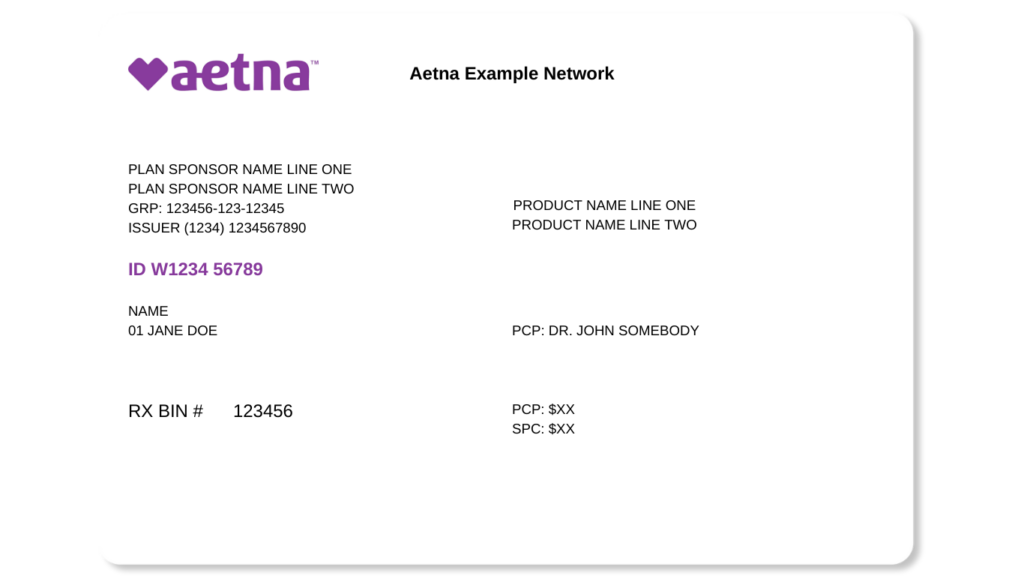
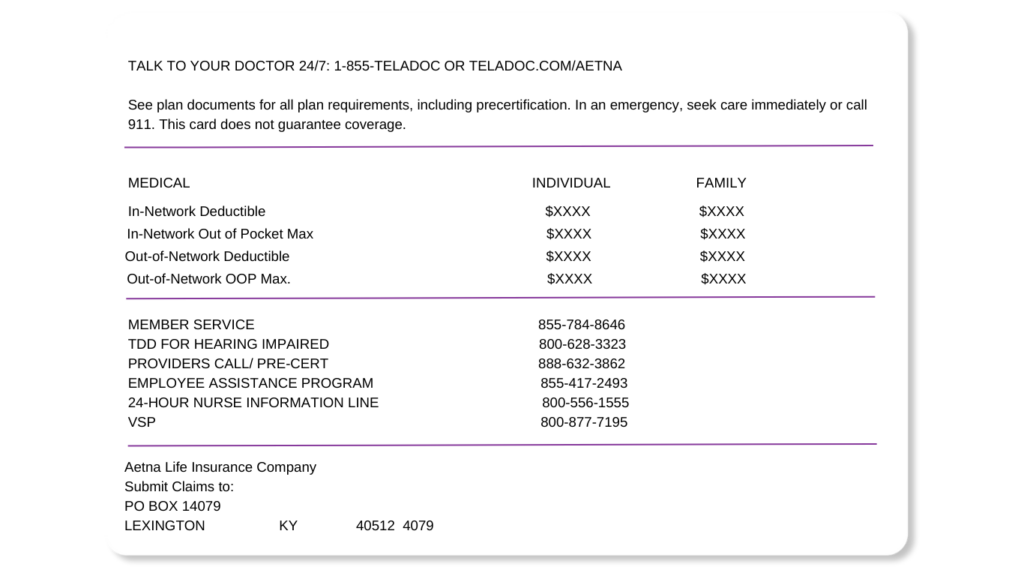
- Review Your Insurance Card: Begin by examining your Aetna insurance card. This should provide you with details on how to reach customer service and access your account online.
- Aetna Member Website: After registering and logging in to the Aetna member website (usually found on the back of your insurance card), you can access detailed information about your plan, including coverage details, deductibles, and copayments.4
- Summary of Benefits and Coverage Document: Access the Summary of Benefits and Coverage (SBC) document for a comprehensive overview of your plan and its costs. You can find it in your online account or request it from Aetna directly.5
- Customer Service: When calling customer service, have your insurance card and personal information. They can help you understand your coverage, costs, and pre-authorization requirements.
- Speak with Your Employer: If you receive insurance through your employer, your human resources department can provide information on available health plans and assist you in accessing detailed coverage information.
- Consult with Cornerstone’s Admissions Department: Cornerstone is familiar with Aetna’s insurance plans and can assist you in understanding which addiction treatments are covered by your insurance policy.
- Mobile App: Aetna may provide a mobile app for its members to access their plan details, including coverage and claims information, directly from their smartphone.
- Coverage for Specific Treatments: For details on specific treatments, such as addiction services, you should inquire about the types of treatments covered, any network restrictions, and whether you need pre-authorization for services.
- Documentation: It’s important to keep all communications and documents Aetna provides for future reference. This can be helpful in case of a coverage dispute or needing to review specific coverage details.
It’s essential to proactively ask detailed questions to understand your benefits and potential out-of-pocket costs thoroughly.
A comprehensive understanding of your insurance policy can help you make informed decisions about your healthcare and avoid unforeseen expenses.
Are there any restrictions on types of addiction treatment Aetna will pay for?
Aetna provides coverage for a wide range of addiction treatments.
The extent of coverage can vary significantly depending on factors such as the type of plan, individual policy, and other factors.
Some treatments and services may have limitations or exclusions, and it’s important to review your plan to understand what is covered and what is not.
- Experimental or Investigational Treatments: Treatments considered experimental, unproven, or not widely accepted in the medical community might not be covered.
- Certain Medications: Some prescription drugs may not be covered, especially if they are considered “off-label” for treating addiction. Additionally, newer and more expensive medications might be excluded if less costly yet effective alternatives are available.
- Luxury or Executive Rehab Centers: High-end treatment facilities that offer luxury amenities often come with higher costs that may not be fully covered by insurance.
- Holistic or Alternative Therapies: Treatments like acupuncture, massage therapy, or herbal supplements, often considered alternative or complementary therapies, might not be covered.
- Long-Term Residential Treatment: While inpatient treatment is often covered, there might be limits on the length of stay that Aetna will cover in a residential treatment facility.
- Out-of-Network Providers: If you choose to receive medical treatment from a healthcare provider or facility outside Aetna’s network, you may have to bear higher costs, or your plan may not cover the service. However, this solely depends on the type of Aetna plan you have. Some Aetna plans have provisions for covering out-of-network providers without any issues.
- Private Detox Facilities: Some private detox programs may not be fully covered, especially those offering more comfortable or luxurious settings.
- Non-essential Amenities: Insurance may not cover services deemed non-essential to recovery, such as private rooms, special food, or recreational activities.
- Over-the-Counter Substances: Even if recommended for treatment (like specific vitamins or supplements), over-the-counter products may not be covered.
How soon can I get into rehab with Aetna coverage?
If you have Aetna insurance coverage, you can usually get into rehab within a few days.
Please get in touch with us today, and we can provide you with a better understanding of the steps you need to take to get admitted to our substance abuse treatment program.
What if I can't cover my deductible?
If you’re struggling to afford your Aetna deductible, you have options.
One option is requesting a hardship exception from Aetna.
Here’s what else you can do:
- Contact Aetna for a Hardship Exception: It’s best to contact Aetna directly to discuss any financial hardships you may face. Depending on your situation, they may offer special considerations or hardship exceptions. They can guide you through the application process for these exceptions.
- Payment Plans: If you are having trouble making a one-time payment for your healthcare, you can inquire about setting up a payment plan. Aetna or your healthcare provider may be able to arrange a monthly payment schedule that suits your needs. Cornerstone is also willing to consider payment plans on a case-by-case basis. To get started, please get in touch with admissions.
- Health Savings Account (HSA) or Flexible Spending Account (FSA): Use funds from an HSA or FSA to pay your deductible. Contributions to these accounts are pre-tax and can be used for qualified medical expenses.6
- Negotiate Charges: Consider negotiating the cost of healthcare with your provider, especially if paying out of pocket. They may offer discounts or reduced rates.
- Financial Assistance Programs: Check if the hospital or treatment center has financial assistance or charity care programs that reduce or waive some costs for eligible individuals.
- Community Clinics and Health Centers: Seek care from local community health clinics or centers that offer services based on a sliding scale related to your income.
- Charity Care: Consider researching charities that specifically help those with medical expenses, as they assist individuals struggling to pay for healthcare.
- Understand Your Policy: It’s important to review your insurance policy thoroughly and determine what preventative care is covered under it and may not be subject to the deductible.
- Catastrophic or High-Deductible Health Plans: If you’re facing significant medical costs with your high-deductible health plan, check if you qualify for a catastrophic plan or other special enrollment options with lower deductibles.
Sources
- About Us & Company Information | Aetna, https://www.aetna.com/about-us.html
- Substance Use Disorder Screening Tools & Resources | Aetna, https://www.aetna.com/health-care-professionals/patient-well-being/substance-use-screening-tools-resources.html
- How Aetna Can Help You With Substance Use Disorder, https://www.aetna.com/health-guide/substance-use-disorder.html
- Member Login & Register | Aetna, https://www.aetna.com/individuals-families/using-your-aetna-benefits/secure-member-account.html
- Medical Clinical Policy Bulletins, https://www.aetna.com/health-care-professionals/clinical-policy-bulletins/medical-clinical-policy-bulletins.html
- What Is An HSA & What Can It Be Used For? | Aetna, https://www.aetna.com/health-guide/can-pay-hsa.html
CLINICALLY REVIEWED

Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, our Clinical Director is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address the underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.