Cornerstone
UMR SUBSTANCE ABUSE TREATMENT
Learn about UMR drug rehab coverage and get help at our Arizona rehab centers that accept UMR's policies
UMR DRUG TREATMENT COVERAGE
Beginning your recovery journey starts with knowing your treatment options, and UMR’s drug rehab coverage plays a vital role in accessing essential care.
At Cornerstone Healing Center, we are proud to accept UMR insurance, allowing us to provide comprehensive substance abuse treatment programs to those needing help.
We are committed to a personalized approach to care, blending evidence-based and holistic therapies to promote healing and sustainable recovery.
Let us walk you through the specifics of UMR coverage, our programs, and how we can collaborate to help you achieve a healthier, substance-free future!
Jump to the following
View our addiction treatment locations
Addictions we treat at Cornerstone
UMR COVERED DRUG REHAB PROGRAMS

Our Residential Treatment Programs offer comprehensive and continuous support to individuals who are struggling with substance abuse. We use a combination of detoxification, counseling, and holistic practices to promote healing. Our evidence-based therapies include Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), and we also integrate mindfulness, yoga, and nutrition therapy. Our primary objective is to assist individuals in addressing the underlying causes of addiction and provide them with effective tools to maintain long-term recovery and prevent relapse.

Our Partial Hospitalization Programs (PHP) are specifically designed to help individuals struggling with substance abuse. The program provides a comprehensive and structured approach to recovery, with intensive daytime treatment that includes therapy, group sessions, and holistic practices. The program runs five days a week for six hours daily, allowing individuals to receive treatment without requiring overnight stays. This approach is designed to help individuals identify and address their addiction while equipping them with the necessary skills and support to maintain long-term sobriety. PHP emphasizes accountability and encourages individuals to apply what they have learned in real-world situations.

Our Intensive Outpatient Program (IOP) is the initial phase of the treatment process, followed by the standard Outpatient Program that runs three days a week with a flexible schedule to cater to personal commitments and responsibilities. These Outpatient Programs offer a range of therapeutic activities, including individual counseling, group therapy, and skill development workshops. Our comprehensive approach ensures a supportive pathway towards healing and rebuilding the lives of those affected by addiction.
UMR Health Insurance
UMR is a third-party administrator (TPA) of health insurance plans operating as a part of UnitedHealthcare.1 It provides flexible and customized administrative services to self-insured companies, managing various health plans and benefits. With a history of focusing on cost-effective solutions and personalized care management, UMR aims to optimize healthcare benefits while controlling expenses. Its coverage options are extensive, encompassing a wide range of medical, dental, and vision care services tailored to meet the diverse needs of its members. UMR’s approach emphasizes accessibility, quality care, and comprehensive support to ensure the well-being of its beneficiaries.
ABOUT UMR DRUG TREATMENT COVERAGE
UMR health insurance provides coverage for substance abuse treatment, supporting a broad spectrum of services to aid in recovery. This includes inpatient and outpatient care, detoxification programs, therapy sessions—both individual and group—and various rehabilitative services.2 By offering access to a range of evidence-based treatments and holistic approaches, UMR aims to address the multifaceted needs of individuals struggling with addiction. Coverage specifics, such as the extent of care and the types of programs covered, can vary based on the policyholder’s plan, emphasizing the importance of personalized treatment plans and comprehensive support for long-term recovery.
Alumni Client Family Testimonial
I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does UMR Provide Coverage For?
Addictions Covered by UMR
UMR policies provide extensive coverage for substance abuse disorders, including treatment for alcohol and drug rehabilitation. The following are examples of addictions treated at our Arizona facilities, which are typically covered by your UMR health insurance:
- Alcohol: Holistic programs aimed at alcohol addiction recovery are supported by UMR insurance.
- Opioids: UMR offers comprehensive care and assistance for those battling opioid addiction.
- Fentanyl: Treatments for fentanyl addiction, along with specialized care and support, are included under UMR coverage.
- Cocaine: UMR covers specific treatment plans designed to address cocaine dependency and promote lasting sobriety.
- Methamphetamine: UMR insurance backs treatment for meth addiction, with a focus on addressing the fundamental issues for successful recovery.
- Benzodiazepine: Programs targeting benzodiazepine withdrawal and rehabilitation receive coverage from UMR.
- Co-Occurring Disorders: Therapy customized for individuals with simultaneous addiction and mental health diagnoses is covered by UMR insurance.
Programs We Offer
Understanding Your umr Health Insurance Card
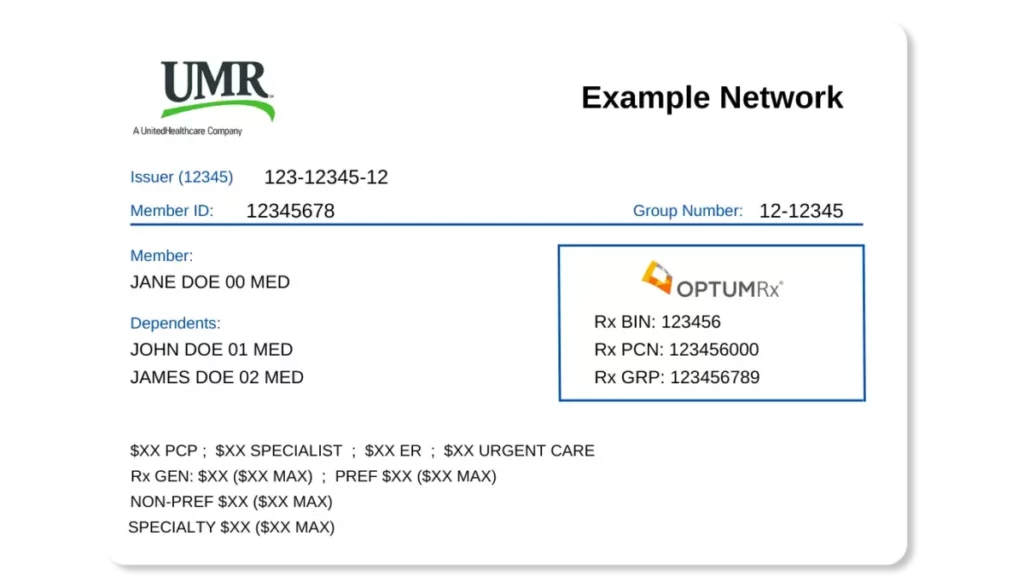
UMR Card Front
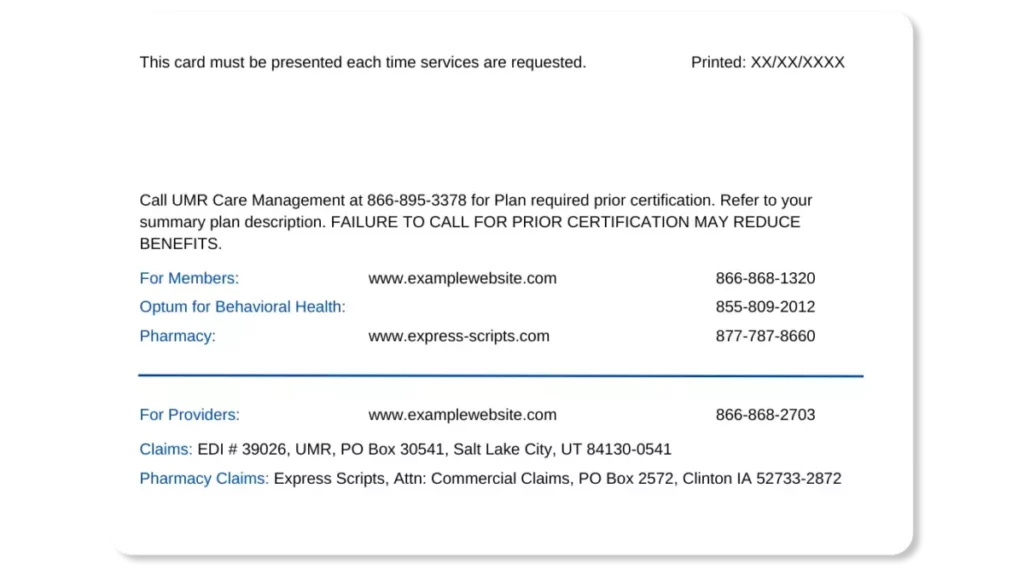
UMR Card Back
Meet Our Clinical Team
Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.
Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About UMR
Get answers to the most commonly asked questions about UMR rehab coverage.
UMR health insurance covers a comprehensive range of substance abuse treatments to support recovery, including:
- Detoxification Services: Medical detox to safely manage withdrawal symptoms under professional supervision.3
- Inpatient Rehabilitation: Residential care providing 24/7 support and therapy for individuals in a controlled environment.
- Outpatient Programs: Including standard outpatient treatment and Intensive Outpatient Programs (IOPs) that allow patients to live at home while receiving treatment.
- Partial Hospitalization Programs (PHPs): Day programs offering intensive treatment without overnight stays, serving as a middle ground between inpatient and outpatient care.
- Counseling Services: Individual and group counseling sessions to address psychological aspects of addiction.
- Therapy Sessions: Including Cognitive-Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and other evidence-based therapies.
- Medication-Assisted Treatment (MAT): Utilizing medications in combination with counseling and behavioral therapies for a holistic approach to substance abuse treatment.
- Support Groups: Facilitated group meetings that provide peer support and encouragement throughout recovery.
- Treatment for Co-Occurring Disorders: Specialized care for individuals with concurrent mental health issues and substance abuse disorders.
The extent of coverage for these treatments can vary based on the specifics of your UMR policy, including plan type and any applicable deductibles or co-pays.4
Insurance providers and third-party administrators often require pre-authorization for certain healthcare services, such as drug and alcohol rehabilitation.5
Pre-authorization, also known as prior authorization, is when the insurer or administrator assesses the medical necessity of a proposed treatment plan and confirms that the coverage aligns with the insurance policy. This evaluation usually occurs before the treatment begins.
We understand that dealing with insurance requirements and pre-authorizations can be overwhelming. Fortunately, we offer assistance with submitting these requirements. Our team of experts can help alleviate some of the burden of treatment and navigating insurance stipulations. Please submit your insurance verification to get support to begin the process.
The duration of drug and alcohol rehabilitation coverage provided by UMR insurance may vary depending on several factors, such as the patient’s insurance policy and medical professionals’ evaluation of treatment needs.
UMR health insurance policies offer a wide range of addiction treatment programs, including inpatient or residential care, outpatient services, detoxification programs, and medication-assisted therapy.
To determine the length of time your UMR policy covers drug rehab, you should review your individual insurance plan and speak with our admissions team. Our team of admissions experts can assist you in understanding the addiction treatment services covered by UMR and determine your insurance coverage level.
UMR offers coverage for a variety of addiction treatments.
The extent of coverage depends on the specific terms, limitations, and exclusions of your policy, as well as the medical necessity and outcomes of any previous treatments.6
Consider the following key factors:
- Annual and Lifetime Caps: Some policies may restrict the frequency of substance abuse treatment within a year or across the policy’s lifespan. Examining your plan for any specified limits on treatment episodes or days covered is crucial.
- Medical Necessity: UMR generally requires a determination of medical necessity for each treatment episode, meaning that a healthcare professional must verify the essential nature of the treatment for your recovery.
- Outcome of Prior Treatment: Coverage for additional treatment sessions often considers the effectiveness and progress of any previous treatment, focusing on the need and potential benefits of further treatment.
- Treatment Modality: The type of treatment you’re pursuing impacts coverage; for instance, UMR might more consistently cover outpatient therapy sessions annually than multiple inpatient rehab stays.
- Specific Policy Details: Grasping the specifics of your UMR plan is vital, as policies vary greatly in their coverage for repeated treatments.
- Pre-Authorization Requirement: Similar to initial treatments, subsequent treatments typically require pre-authorization from UMR to confirm eligibility for coverage and medical necessity.
To understand coverage for addiction treatments, review your UMR policy, contact Cornerstone to verify your insurance benefits, or consult a UMR representative for details on coverage for repeated treatment.
At Cornerstone Healing Center, we understand that the timeline for beginning addiction treatment can vary depending on the individual’s needs.
To get started, contact us directly.
Our team will evaluate your needs, verify your UMR insurance benefits, and handle all the specifics of your admission.
Our goal is to assist you at every step and ensure you can start your journey to recovery as soon as possible!
Sources
CLINICALLY REVIEWED
Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.

Get Started
Now
Call and speak with one of our caring team members about help for you or a loved one.






















