Cornerstone
TRIWEST SUBSTANCE ABUSE TREATMENT
Learn about TriWest drug rehab coverage and get help at our Arizona rehab centers that accept TriWest's policies
TRIWEST DRUG TREATMENT COVERAGE
Knowing your options is the first step to recovery, and TriWest’s drug rehab coverage helps connect you to essential care.
At Cornerstone Healing Center, we’re honored to accept TriWest insurance, enabling us to offer comprehensive substance abuse treatment programs to those seeking help.
Our approach to care is personalized, blending evidence-based and holistic therapies to promote healing and sustainable recovery.
Let’s discuss the details of your TriWest coverage and the different treatment options we offer. We’ll then work together to create a plan that helps you build a healthier life free from substance abuse!
Jump to the following
View our addiction treatment facilities
Addictions we treat at Cornerstone
TRIWEST COVERED DRUG REHAB PROGRAMS

Our Residential Treatment Programs offer all-encompassing and ongoing assistance for those battling substance abuse. We blend detoxification, therapeutic counseling, and holistic healing techniques. Our treatments are grounded in proven methodologies such as Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), enriched with practices like mindfulness, yoga, and nutrition therapy. Our objective is to uncover and tackle the root causes of addiction, providing individuals with the necessary strategies for enduring recovery and preventing relapse.

Our Partial Hospitalization Programs (PHP) provide a comprehensive, structured recovery plan. They operate five days a week for six hours daily and offer intense daytime care, including therapy, group sessions, and holistic practices. The programs do not require overnight stays. This approach helps participants identify and overcome their addiction while gaining essential skills and support for long-term sobriety. The PHP model emphasizes personal responsibility and encourages participants to apply their new insights to everyday situations.

Our Intensive Outpatient Program (IOP) is the first step toward recovery. It is followed by our Standard Outpatient Program, which runs three times a week. This program is designed to be flexible, accommodating personal obligations. Both programs offer a range of therapeutic interventions, including one-on-one counseling, group therapy, and developmental workshops. Our holistic approach provides a nurturing journey toward recovery to restore the lives of those affected by addiction.
TriWest Health Insurance
TriWest Healthcare Alliance is a health insurance provider primarily focusing on veterans, military personnel, and their families. The company holds government contracts with the Department of Veterans Affairs (VA) to provide various healthcare services, including hospital visits, outpatient care, mental health services, and specialty care.1 TriWest was established to bridge the gap between military and civilian healthcare systems, and it is committed to ensuring that those who served in the military have access to high-quality healthcare. The services provided by TriWest are an essential part of the VA’s efforts to offer comprehensive and accessible care to the veteran population across the United States.
About TriWest drug treatment coverage
TriWest health insurance offers comprehensive coverage for substance abuse treatment tailored specifically for veterans and military families. This coverage includes a wide range of services aimed at substance abuse recovery, such as detoxification, inpatient and outpatient rehabilitation, therapy sessions, and support groups.2 By working in collaboration with the Department of Veterans Affairs, TriWest ensures that veterans receive the necessary care and support to overcome substance abuse issues. The company focuses on personalized treatment plans to address the unique needs of each individual, emphasizing its dedication to the well-being and long-term recovery of veterans struggling with substance abuse.
Alumni Client Family Testimonial
“I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does TriWest Provide Coverage For?
Addictions Covered by TriWest
TriWest policies provide extensive coverage for substance abuse disorders, encompassing alcohol and drug rehabilitation. Below are several addictions treated at our Arizona facilities, which are typically covered by your TriWest health insurance:
- Alcohol: Our holistic programs for alcohol addiction recovery are supported by TriWest insurance.
- Opioids: TriWest offers thorough care and assistance for individuals recovering from opioid addiction.
- Fentanyl: Treatments for fentanyl addiction, including specialized support, are covered by TriWest insurance.
- Cocaine: TriWest insurance includes coverage for specialized treatment plans aimed at overcoming cocaine dependency and achieving long-lasting sobriety.
- Methamphetamine: Support for methamphetamine addiction treatment, with a focus on addressing the fundamental issues for successful recovery, is provided by TriWest insurance.
- Benzodiazepine: Programs for benzodiazepine withdrawal and rehabilitation are included under TriWest coverage.
- Co-Occurring Disorders: TriWest coverage extends to personalized therapy for individuals dealing with both addiction and mental health challenges.
Programs We Offer
MEET OUR CLINICAL TEAM
Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.
Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
Frequently Asked Questions
Get answers to the most commonly asked questions about TriWest substance abuse treatment coverage
What types of drug rehab programs does TriWest Health cover?
TriWest provides extensive coverage options for individuals struggling with substance abuse, with a focus on immediate medical assistance and a sustainable path to recovery.3
Below is an overview of the services provided by TriWest:
- Emergency and Planned Inpatient Services: Covers both emergency and non-emergency hospital stays to ensure timely access to necessary care.
- Intensive Outpatient Programs (IOPs): For those requiring consistent monitoring without 24/7 hospitalization, including group therapy, individual counseling, and structured recovery activities.
- Detox Services: Supports managing withdrawal symptoms safely under medical supervision, facilitating a smoother recovery process.
- Mental Health Services: Addresses co-occurring mental health conditions with treatments like cognitive-behavioral therapy (CBT) and psychotherapy, recognizing the intricate link between addiction and mental health.
- Partial Hospitalization Programs (PHPs): Offers a middle ground between inpatient care and outpatient services, providing intensive treatment without an overnight stay.
- Residential Treatment Programs: For individuals needing continuous care in a residential environment, encompassing medical oversight, therapy, and peer support.
TriWest’s comprehensive coverage facilitates a holistic approach to substance abuse treatment, empowering military members and their families to embark on a personalized recovery journey.
Will TriWest cover my stay in drug rehab?
TriWest typically provides coverage for addiction treatment stays, though the extent of coverage can vary significantly based on your policy, the required type of treatment, and other factors.4
It’s important to understand the fundamental aspects of your insurance coverage, which include:
- Treatment Types: TriWest supports inpatient and outpatient treatments, encompassing detoxification, residential care, and necessary medical interventions for inpatient services. Outpatient services include therapy sessions, group counseling, and partial hospitalization programs.
- Pre-Authorization Requirement: Many treatments necessitate pre-authorization from TriWest, requiring approval before commencement to ensure coverage.
- Choosing Providers: Opting for in-network providers generally guarantees fuller coverage with TriWest, as it operates with a network of preferred providers. Services from out-of-network providers may still be covered but at a reduced rate, subject to the details of your plan.
- Understanding Deductibles and Co-pays: It is essential to familiarize yourself with your deductibles and co-pays, as they will affect your out-of-pocket treatment costs.
- Coverage Duration: Policy specifications will dictate the length of coverage for inpatient stays or the allotment of outpatient sessions.
- Type of Addiction: The nature of the substance or behavior being treated can influence coverage, with certain plans imposing specific limitations or exclusions for various types of addiction.
- Ongoing Treatment Review: The necessity for continued treatment is regularly evaluated to ascertain its medical necessity, which influences the coverage duration.
Understanding these factors can help you better understand your insurance coverage for addiction treatment from TriWest.
Reviewing your policy in detail or consulting with a healthcare professional is recommended to navigate and comprehend your specific coverage nuances.
At Cornerstone, we can help you determine your benefits by verifying your insurance coverage and clarifying any uncertainties about what is and isn’t covered.
How do I determine my policy coverage?
Finding out exactly what your TriWest insurance policy covers can be a straightforward process if you follow these steps:
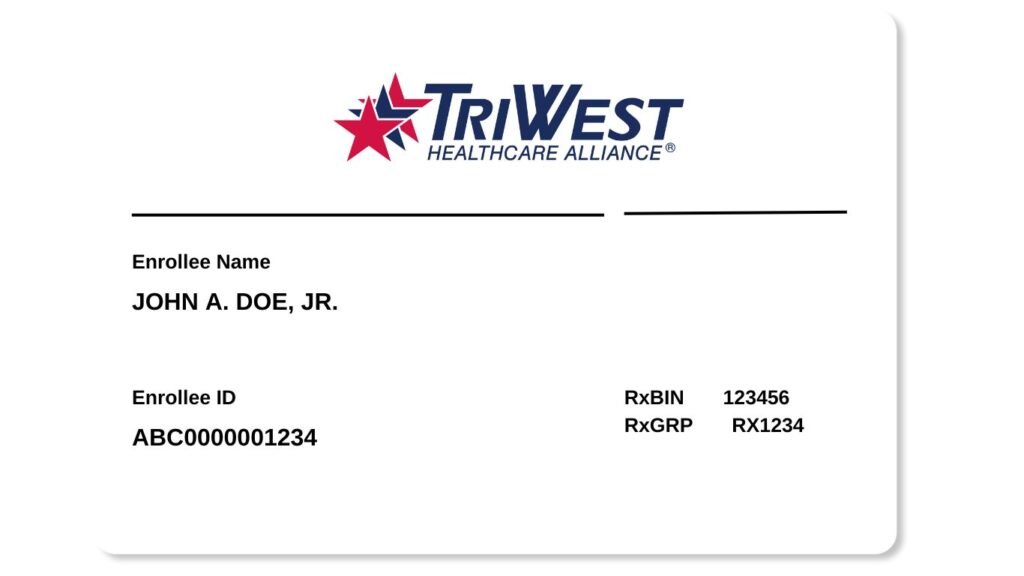
- Review Your Insurance Card: Begin by locating your TriWest insurance card. This will have important information such as your policy number and contact details for customer service.
- Log In to Your TriWest Account: Visit the TriWest website and log into your account. You’ll need to register using your policy details if you haven’t set up an account yet.
- Review Policy Documents: Once logged in, access your policy documents. These documents provide detailed information about your coverage, including benefits, exclusions, and limitations.
- Check the Summary of Benefits: Look for a summary of benefits, which outlines the key aspects of your coverage in an easy-to-understand format. This summary will include information on types of covered services, deductibles, co-pays, and out-of-pocket maximums.
- Search for Specific Services: Use the website’s search feature or navigate the menus to find information on specific services, such as substance abuse treatment, to see what your policy covers.
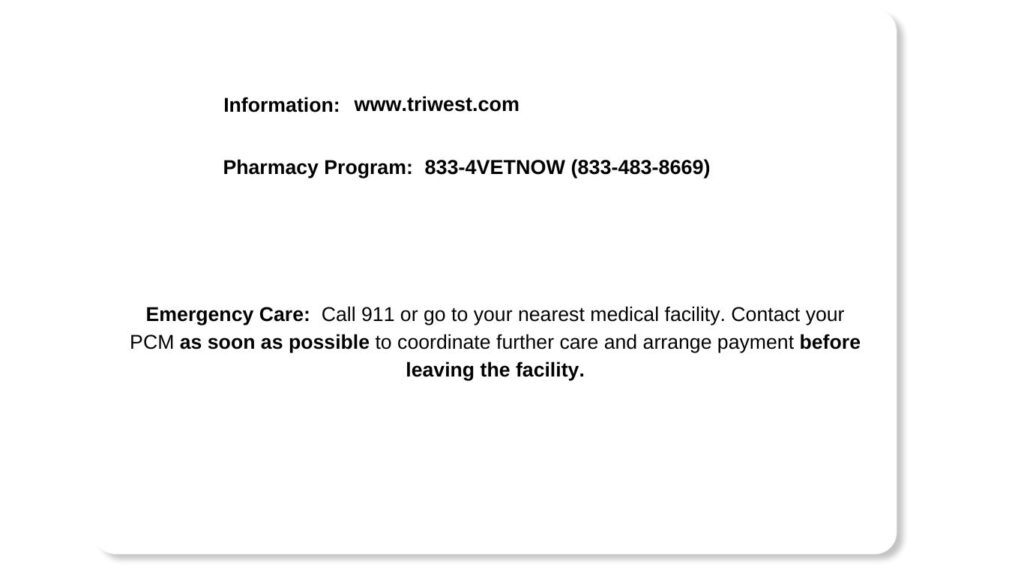
- Contact Customer Service:If you have questions or need clarification, call your insurance card’s TriWest customer service number. Be ready with your policy number and specific questions about your coverage.
- Consult with Healthcare Providers: Speak with healthcare providers who are in the TriWest network. They can provide insights into what treatments are typically covered and assist with pre-authorization.
- Pre-Authorization: For certain services, you might need pre-authorization. If necessary, find out how to initiate this process for your treatment.5
- Understand Appeals and Grievances: Familiarize yourself with the process for filing an appeal or grievance if a claim is denied or you disagree with a coverage decision.
- Stay Informed About Changes: Keep an eye on any updates or changes to your policy. TriWest may send updates through mail, email, or your online account.
Will TriWest pay for rehab more than once?
If you’re concerned about needing multiple stays in rehab, it’s good to know that TriWest insurance generally allows for this as long as each treatment is considered medically necessary. While nobody plans on multiple treatment episodes, addiction is often a chronic condition that may require ongoing care. Keeping a few things in mind when using your TriWest insurance for more than one rehab stay is important.
First, you’ll need to check the specifics of your policy to see if there are any limitations on the number of treatments you can undergo or any time restrictions between treatments. While TriWest generally supports ongoing care, insurance policies can differ in their particulars.
For the most accurate and personalized information, we recommend consulting with TriWest directly or allowing our admissions team to verify your insurance coverage. By doing so, you’ll clearly understand what your plan covers, how many treatment episodes are included, and whether you should be aware of any out-of-pocket costs.
So, yes, you can absolutely utilize your TriWest insurance multiple times for rehab if it’s medically necessary. This flexibility helps ensure you have the coverage you need to fully engage in your recovery journey, no matter how long it takes. Always remember to verify the specifics of your policy to make informed decisions.
Are there any limits on types of addiction treatment TriWest will pay for?
TriWest insurance offers broad coverage for many types of substance abuse treatments, supporting various approaches to recovery. This typically includes established and evidence-based treatments like inpatient care, outpatient programs, detox services, and behavioral therapies.
However, it’s essential to understand that while TriWest has a comprehensive approach to treating addiction, there may be some limitations. For example, experimental or less conventional treatments—such as specific holistic therapies or newer, non-FDA-approved medications—may not be covered by your policy.6
So, what should you do to navigate these limitations? The most effective strategy is to get the specifics before treatment begins. You can do this by consulting directly with TriWest to confirm what treatments are covered under your policy. Alternatively, our admissions team at Cornerstone can assist you in verifying your insurance coverage, helping to ensure that you’re making choices that align with your medical needs and insurance benefits.
By being proactive and checking your coverage details, you can enter treatment with a clearer mind, free from the stress of unexpected financial commitments. Knowing what your insurance covers will let you focus on what’s most important: your path to recovery.
How soon can I get into rehab with TriWest coverage?
We understand that time is critical in addiction treatment. Therefore, we have simplified our admissions process to quickly get you into the right program.
After verifying your active TriWest insurance and the treatments it covers, we will promptly initiate your recovery journey. Our team will work closely with TriWest to handle all the necessary paperwork and approvals, cutting through the red tape for you. We aim to minimize waiting periods so you can start your treatment as soon as possible, often in days or hours, depending on your situation.
With TriWest’s coverage and our expedited admissions process, you won’t have to put your life on hold while waiting for treatment. Instead, you can begin your path to recovery sooner than you might have thought possible. Taking swift action can be crucial, especially when immediate intervention is necessary.
Sources
CLINICALLY REVIEWED

Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.

Get Started
Now
Call and speak with one of our caring team members about help for you or a loved one.