Cornerstone
Cigna Substance Abuse Treatment
Learn about Cigna drug rehab coverage and get help at our Arizona rehab centers that accept Cigna's policies
Cigna Drug Treatment Coverage
We are eager to announce that Cigna insurance is available at Cornerstone Healing Center, which means we can provide our substance abuse treatment programs to those seeking help!
Our goal is to offer personalized, high-quality care that combines proven treatments with holistic therapies, promoting healing and long-term success in recovery.
Let us guide you through the details of your Cigna coverage, provide information about our programs, and work together to help you build a healthier, substance-free future.
Your journey toward recovery starts with exploring your options, and we believe that Cigna’s coverage for drug rehab can be the lifeline you need to get the care you deserve.
Jump to the following sections
View our addiction treatment locations
Now Accepting AHCCCS Health Choice,
Mercy Care, TriCare, and Triwest
Addictions we treat at Cornerstone
Cigna Covered Drug Rehab Programs

Our Residential Treatment Programs offer extensive and ongoing assistance to those dealing with substance abuse issues. We combine detoxification, counseling, and holistic approaches to foster recovery. Our treatments are grounded in proven methods such as Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), enriched with mindfulness, yoga, and nutrition classes. Aimed at tackling the root causes of addiction, we strive to provide individuals with the necessary skills for lasting recovery and prevention of relapse, all under the coverage options available through Cigna insurance.

Our Partial Hospitalization Programs (PHP) for substance abuse deliver an all-inclusive and organized recovery strategy supported by Cigna insurance. Operating five days a week, six hours each day, our PHP offers intensive daytime care that encompasses therapy, group activities, and holistic methods, all without the need for overnight accommodation. This model assists participants in confronting and managing their addiction, equipping them with vital skills and support for enduring sobriety. The program stresses the importance of accountability and motivates participants to implement the recovery techniques they've acquired into their everyday lives.

Our Intensive Outpatient Program (IOP) serves as the initial phase, succeeded by our standard Outpatient Program, available three days a week with adaptable scheduling to fit personal obligations and duties. Covered by Cigna insurance, these Outpatient Programs feature a range of therapeutic interventions, such as individual counseling, group therapy, and skill-building workshops. This holistic strategy offers a nurturing route towards recovery and the restoration of lives impacted by addiction.
Cigna coverage for drug and alcohol rehab
Cigna is a prominent global health service company established in 1982 due to a merger between INA (1792) and CG (1865).1 The company offers various health insurance options, with comprehensive coverage for substance abuse treatments, which signifies its dedication to providing accessible and effective care for addiction. Cigna’s focus on personalized, evidence-based treatment plans encourages recovery and overall well-being. By emphasizing mental health and addiction, Cigna’s holistic approach to healthcare benefits individuals and communities worldwide.
ABOUT CIGNA DRUG TREATMENT COVERAGE
Cigna is dedicated to promoting comprehensive health and well-being. To fulfill this commitment, it offers coverage for substance abuse treatment, supporting individuals at every stage of their recovery journey. Cigna’s coverage for substance abuse encompasses detoxification, inpatient, residential, and outpatient services, therapy, and counseling.2 By collaborating with a network of qualified providers, Cigna ensures that its members receive tailored and appropriate levels of care. The company’s approach is inclusive, addressing the physical, psychological, and social aspects of addiction to encourage a more sustainable recovery.
Cornerstone Success Stories - Patrick and Nicole
I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does Cigna Provide Coverage For?
Addictions Covered by Cigna
Cigna policies provide comprehensive coverage for drug and alcohol rehabilitation. Below are some addictions treated at our Arizona facilities, which are likely covered by your Cigna health insurance:
- Alcohol: Cigna insurance supports holistic programs for alcohol addiction recovery.
- Opioids: For those tackling opioid addiction, care and support are provided, backed by Cigna's comprehensive coverage.
- Fentanyl: Cigna insurance includes coverage for fentanyl addiction treatment, offering specialized care and support.
- Cocaine: Treatment plans designed to address cocaine dependency and promote long-term sobriety are covered by Cigna.
- Methamphetamine: Cigna insurance aids in treating methamphetamine addiction, targeting the fundamental issues for effective recovery.
- Benzodiazepine: Cigna covers treatment programs for benzodiazepine withdrawal and rehabilitation.
- Co-Occurring Disorders: Cigna provides coverage for personalized therapy for those with dual diagnoses of addiction and mental health issues.
Programs We Offer
Understanding Your Cigna Health Insurance Card

Cigna Example Card Front
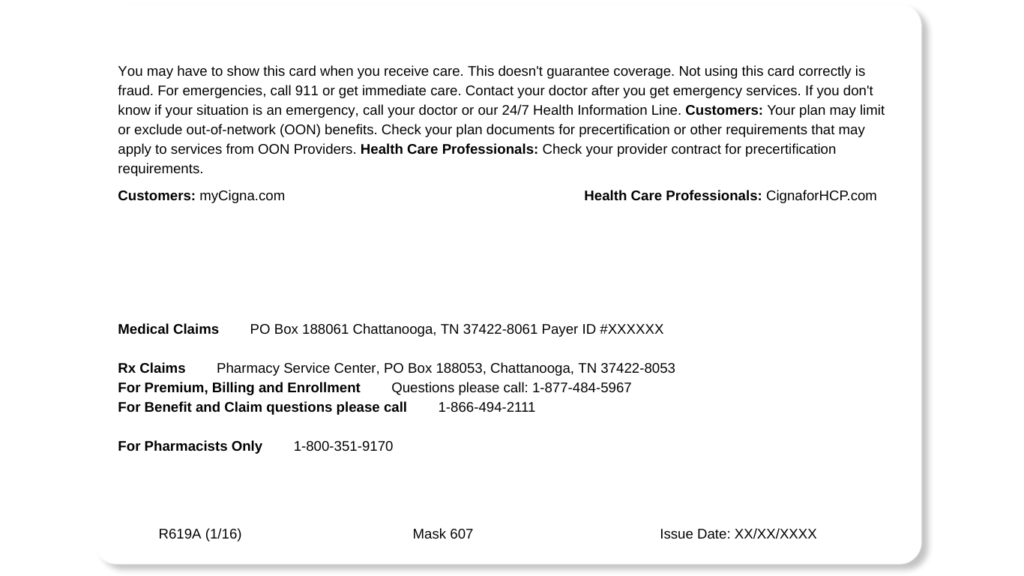
Cigna Example Card Back
MEET OUR CLINICAL TEAM

Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.

Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About Cigna Rehab Coverage
Get answers to the most commonly asked questions about Cigna coverage for substance abuse treatment.
Does Cigna Cover Detox?
Cigna insurance covers detox as part of their many health plan options.
Detox is the first important step to recovery from drug and alcohol abuse.
How much detox is covered and for how long depends on your specific Cigna plan and needs.
It’s extremely important to review your Cigna policy details to fully understand your plan’s detox benefits.
This way, you can use your coverage to the fullest for a safe and successful start to getting sober.
If you need help understanding your Cigna benefits, please verify your insurance details with us; we will gladly assist you.
Does Cigna Cover Inpatient Treatment?
Cigna health plans often cover inpatient rehab as part of their mental health benefits.3
Inpatient rehab with Cigna usually includes important services needed to treat drug and alcohol abuse, like:
- Detox with medical supervision
- Therapy sessions
- Other rehab activities
Your specific Cigna plan determines how long you can stay and what therapies are covered.
It’s important to read over your policy details to fully understand your inpatient rehab benefits and limits.
Let us help you by verifying your insurance coverage.
We can provide you with a clear understanding of your policy coverage so that you know what to expect.
Does Cigna Cover Partial Hospitalization Programs?
Cigna health plans usually cover partial hospitalization programs (PHP) as an essential part of their mental health and substance abuse services.4
PHP coverage includes different types of therapy and necessary medical care.
Cigna’s PHP coverage is meant to bridge the gap between inpatient and outpatient treatment.
It provides a structured setting for treatment but allows patients to go home at night.
How long the PHP lasts and what types of therapy are included depends on your specific Cigna plan details.
Does Cigna Cover Outpatient Programs?
Cigna insurance plans are known to pay for outpatient treatment services. This is a big plus for people in Cigna rehab programs.
Rehabs that take Cigna allow patients to use different outpatient services. These include one-on-one therapy sessions and group counseling.
Cigna drug rehab coverage usually includes intensive outpatient programs. It may also cover partial hospitalization, depending on the plan.
The same goes for people looking for Cigna alcohol rehab options. Outpatient treatment is an important part of recovery.
It’s good to check with the specific rehab center that takes Cigna. This way, you can confirm how much outpatient treatment coverage you have.
Do I Have to Go an In-Network Cigna Treatment Center?
You don’t have to go to a Cigna in-network rehab if you don’t want to.
But it’s good to know the pros and cons of choosing a Cigna drug and alcohol rehab in their network.5
Benefits of Going In-Network
- Lower Costs: Rehabs in Cigna’s network usually cost you less because they have special deals with Cigna.
- Easy Billing: Cigna rehabs in the network often have simple billing and insurance claim processes.
- Lots of Coverage: In-network centers typically offer many Cigna-covered services, from detox to intensive outpatient care.
- Pre-Checked Services: Cigna has already checked that they will cover services at in-network rehab centers. This means less chance of denied claims.
Cons of Going In-Network
- Fewer Choices: You may have limited options for treatment centers because you can only choose from Cigna’s network.
- Possible Wait Times: Popular in-network Cigna drug rehab centers might have longer wait times.
- Location Limits: Some areas have many in-network options, so you may have to travel for treatment.
- Basic Approaches: In-network rehabs might only offer standard treatment options that Cigna covers, nothing extra.
What About Going to an Out-of-Network Treatment Center?
Pros of Going Out of Network with Cigna
- More Rehab Options: Going out of network means you have more rehab centers to choose from, including special ones that focus on specific things.
- Unique Treatments: Out-of-network Cigna rehab centers may offer new or special treatments that are not available at in-network places.
- Care Just for You: Out-of-network centers can often give you care that’s made just for your needs.
- Cutting-Edge Therapies: These centers might have the latest therapies and programs that in-network places still need.
Cons of Going Out of Network with Cigna
- Higher Costs: Care outside Cigna’s network usually means paying more out of pocket because Cigna may cover less.
- Complex Reimbursement Process: Getting paid back for out-of-network services can be more precise and take longer.
- Uncertainty in Coverage: Knowing what services and treatments Cigna will cover outside their network is harder.
- Limited Insurance Negotiations: When you don’t have access to Cigna’s negotiated rates, you may pay more for healthcare services, and it can be challenging to predict the costs.
Does Cigna Cover Alcohol Rehab?
Yes, Cigna usually covers alcohol rehab.6
This means that people looking for Cigna alcohol rehab centers can expect to get help paying for treatment through their Cigna health insurance plan.
The coverage often includes different treatments and services offered at these rehab centers.
But it’s important for people seeking help to check with the specific Cigna alcohol rehab center.
This way, they can understand what their own Cigna plan will pay for.
It’s important to remember that an individual’s insurance policy and the treatment center’s agreement with Cigna may differ.
Our team at Cornerstone is knowledgeable in reviewing insurance policies and can verify your insurance benefits at no cost to you.
This way, you will know what your insurance does and doesn’t cover, so there are no surprises later in your treatment!
Sources
CLINICALLY REVIEWED

Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.






















