Cornerstone
Ameriben Substance Abuse Treatment
Learn about alcohol and drug treatment coverage and get help at our Arizona rehab centers that accept AmeriBen's policies
Arizona AmeriBen Drug Treatment
Beginning your path to recovery means exploring your options, and AmeriBen offers substance abuse treatment coverage to help you get the necessary care.
At Cornerstone Healing Center, we accept AmeriBen health insurance, which allows us to provide comprehensive substance abuse treatment programs to those seeking help.
We are committed to providing personalized, high-quality care that combines evidence-based and holistic therapies to promote healing and sustainable recovery.
Let us guide you through the details of your health insurance coverage, our programs, and how we can work together to help you achieve a healthier, substance-free life!
Jump to the following sections
View our Arizona treatment centers
Addictions we treat at Cornerstone
AmeriBen Covered Drug Rehab Programs

Our Residential Treatment Programs offer comprehensive and ongoing support to individuals struggling with substance abuse. We combine detoxification, counseling, and holistic practices to facilitate healing. Our evidence-based therapies include Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). Additionally, we incorporate mindfulness, yoga, and art therapy. Our primary goal is to help individuals address the underlying factors of addiction and provide them with effective tools for long-term recovery and relapse prevention.

Our Partial Hospitalization Programs (PHP) for substance abuse are designed to provide a comprehensive and structured approach to recovery. The program operates five days a week for six hours daily, providing intensive daytime treatment, including therapy, group sessions, and holistic practices, without requiring overnight stays. This approach helps individuals identify and address their addiction while providing them with the necessary skills and support to maintain long-term sobriety. PHP emphasizes accountability and encourages individuals to apply what they have learned in real-world situations.

Our Intensive Outpatient Program (IOP) is the first step in the recovery process. After IOP, clients can continue with the standard Outpatient Program, which runs three days a week and has a flexible schedule to accommodate personal commitments and responsibilities. Our Outpatient Programs offer a range of therapeutic activities, including individual counseling, group therapy, and skill development workshops. We take a comprehensive approach to ensure a supportive pathway to healing and rebuilding lives affected by addiction.
AmeriBen Health Insurance
AmeriBen, based in Meridian, Idaho, has been a prominent Third-Party Administrator since it started in 1958. They began processing medical claims in 1964 and specialize in managing complex benefit plans. As an insurance company, they service over 170 self-funded employer groups and university plans, affecting over one million members. Known for its industry expertise, AmeriBen partners with top-tier networks and vendors, providing advanced technology and sophistication like a large carrier while preserving the personalized service and flexibility of a TPA. The company’s mission goes beyond mere benefits administration; they are committed to significantly impacting lives.1
About AmeriBen Drug Treatment Coverage
AmeriBen Health Insurance is known for its comprehensive coverage in substance abuse treatment. It offers a range of services designed to support recovery and overall well-being. Its plans usually cover inpatient and outpatient treatments, including detoxification, therapy, and counseling. AmeriBen is dedicated to providing accessible care that is tailored to individual needs. Special programs often focus on holistic recovery methods crafted to help individuals regain control over their lives in a supportive and nurturing environment. This demonstrates their commitment to fostering long-term recovery and health.2
Alumni Client Family Testimonial
I feel like Cornerstone gave him all the right tools. He knew how to do it. It was something we could have never done. I just could totally see kind of a personality change in him of wanting, and knowing, that he could achieve and do higher things and greater things. That has to be the people (at Cornerstone).”
Nicole A. - Mother of a Cornerstone Alumni
What Addictions Does AmeriBen Provide Coverage For?
Addictions Covered by
AmeriBen
AmeriBen health insurance provides extensive coverage for substance abuse disorders, including treatment for alcohol and drug rehabilitation.
Below are some of the addictions treated at our Arizona facilities that are likely covered by your AmeriBen health insurance coverage:
- Alcohol: Holistic programs for alcohol addiction recovery are included under insurance policies.
- Opioids: AmeriBen offers comprehensive care and support for those overcoming opioid addiction.
- Fentanyl: Treatment for fentanyl addiction, along with specialized care and support, is available through their insurance.
- Cocaine: AmeriBen insurance covers specialized treatment plans aimed at combating cocaine dependency and promoting sustained sobriety.
- Methamphetamine: Support for meth addiction treatment, which addresses core issues for effective recovery, is provided by AmeriBen insurance.
- Benzodiazepine: AmeriBen insurance includes treatment programs focused on benzodiazepine withdrawal and rehabilitation.
- Co-Occurring Disorders: AmeriBen provides coverage for tailored therapy for individuals diagnosed with co-occurring addiction and mental health conditions.
our Arizona treatment programs covered by AmeriBen
Understanding Your Card and Using Your Benefits
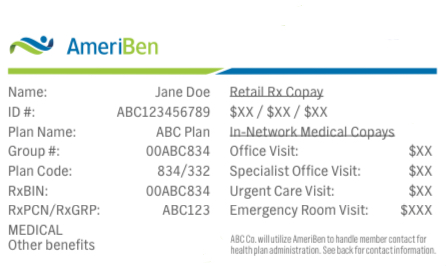
Card Front
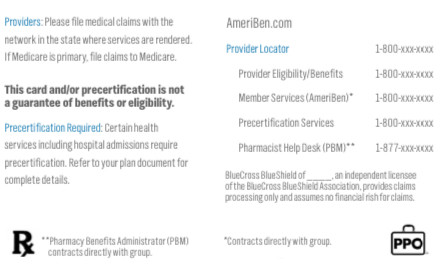
Card Back
Meet Our Clinical Team
Clinical Director of Scottsdale Program
Lionel is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone. Passionate about helping those with addiction and mental health struggles, and he has trained as an EMDR therapist, adopting a trauma-informed approach to find and treat underlying root causes with empathy.
Clinical Director of Phoenix Program
Nate began his recovery journey in 2010 and earned a Master’s in Social Work from ASU. He’s been in the Behavioral Health field since 2013. Specializing in CBT, DBT, and grief, Nate is now the Clinical Director of our Phoenix program, underlined by his passion for helping others who struggled with substance abuse issues as he did.
FAQs About AmeriBen
Substance Abuse Treatment Coverage
Learn about AmeriBen drug treatment coverage for rehab and get answers to commonly asked questions.
What types of drug rehab programs does AmeriBen insurance cover?
AmeriBen health insurance provides comprehensive coverage for addiction treatment programs, giving individuals access to the necessary services for recovery.3
The types of treatment programs covered under AmeriBen substance abuse treatment plans include:
- Detoxification Programs: Covered to help safely manage withdrawal symptoms from drugs or alcohol.
- Inpatient Rehabilitation: Provides 24-hour care and structured treatment environments for intensive recovery support.
- Outpatient Services: Includes therapy and counseling sessions that allow individuals to continue living at home while receiving treatment.
- Partial Hospitalization Programs (PHP): Offers a middle ground between inpatient and outpatient care, providing significant support without full hospitalization.
- Intensive Outpatient Programs (IOP): Focuses on deep, comprehensive treatment that supports recovery while accommodating daily commitments.
- Medication-Assisted Treatment (MAT): Covers medications used to treat substance abuse, counseling, and behavioral therapies.
- Therapy and Counseling: Covers various forms of therapy, including individual, group, and family counseling, to address the psychological aspects of addiction.
- Specialized Programs for Co-Occurring Disorders: Provides integrated treatment for individuals who suffer from concurrent mental health issues along with substance abuse.
It is important for AmeriBen policyholders to review their plans for coverage details, in-network requirements, preauthorizations, and treatment limitations.
Seeking guidance from an AmeriBen agent or medical provider can help address individual needs.
For more information, please complete our confidential insurance verification form to receive a detailed summary of your AmeriBen health insurance benefits and better understand your specific coverage.
How long will AmeriBen cover my stay in rehab?
The length of rehab coverage provided by AmeriBen may vary depending on your health plan’s specifics.
Factors like the type of rehab required, the reason for treatment, and preauthorization requirements are all crucial in determining coverage.
AmeriBen offers up to 90% coverage for most drug and alcohol rehab treatments.
However, the exact percentage of coverage entirely depends on your policy details.
If you have already fulfilled your deductible and maximum out-of-pocket expenses for the year, AmeriBen may cover the entire cost of your rehab treatment.
To understand your coverage clearly, request an insurance verification with us to determine what your policy includes and excludes.
How do I find out what my policy covers?
To find out what your AmeriBen policy covers, follow these straightforward steps:
- Review Your Policy Documents: Start by carefully reading the policy documents you received upon enrollment. These documents provide detailed information about what treatments and services are covered.
- Visit the AmeriBen Website: Log in to your account on the AmeriBen website. Here, you can access specific details about your plan, including coverage limits and exclusions.4
- Contact Customer Service: Call the AmeriBen customer service number provided on your insurance card. A representative can answer specific questions about your coverage and help clarify any uncertainties.
- Request a Summary of Benefits: You can request a detailed summary of benefits, which outlines the coverage specifics, including treatment types and associated costs.
- Consult with Your Healthcare Provider: Discuss the needed treatments with your healthcare provider and have them coordinate with AmeriBen to determine what is covered under your plan.
- Check for Preauthorization Requirements: Some treatments may require preauthorization. Verify if this applies to your intended treatment to ensure coverage.
- Understand Your Deductibles and Out-of-Pocket Maximums: Review how much you’ve already paid towards your deductible and your out-of-pocket maximum, as this will affect how much you’ll potentially pay for covered treatments.
Following these steps will help you fully understand the coverage provided by your AmeriBen health insurance, enabling you to make informed decisions about your healthcare needs.
Are there any restrictions on types of addiction treatment AmeriBen will pay for?
When considering addiction treatment options covered by AmeriBen health insurance, it’s important to be aware of certain restrictions that might apply.
Here are some common limitations:
- Preauthorization Requirements: Some treatments may require preauthorization from AmeriBen before services are rendered to ensure that they are medically necessary.5
- Network Restrictions: To be covered, treatment must often be received from in-network providers, or else you might face higher out-of-pocket costs.
- Type of Treatment Coverage Limits: There may be limits on the types of treatments covered, such as specific exclusions on alternative or experimental therapies.
- Duration of Treatment: Coverage for certain treatments may be limited to a specific duration or number of sessions per year.
- Annual or Lifetime Maximums: Some policies may have annual or lifetime maximum amounts that AmeriBen will pay for addiction treatment services.
- Co-payments and Deductibles: Patients are typically responsible for co-payments and meeting their deductibles before full coverage applies.
- Specific Drug Formulations: Coverage might be limited to specific drug formulations and exclude others, particularly in medication-assisted treatments.
Understanding these restrictions will help ensure that you can effectively plan to access the necessary treatment within the scope of your AmeriBen health insurance coverage.
How soon can I get into rehab with AmeriBen coverage?
If you have AmeriBen health insurance, you can usually start rehab within a few days.
Please get in touch with us today, and we’ll guide you through the necessary steps for admission to our substance abuse treatment program.
Sources
CLINICALLY REVIEWED

Lionel Estrada, LISAC
CLINICAL DIRECTOR
Lionel, our Clinical Director is a Licensed Independent Substance Abuse Counselor (LISAC) with over 4 years at Cornerstone, specializes in addiction and mental health. Trained in EMDR therapy, he employs a trauma-informed, empathetic approach to address the underlying causes of these issues.
- Read our Editorial Policy
Still have questions about treatment?
Our admissions specialists are here to explain the process, answer any questions you may have, and ensure you’re getting the help you need to live a healthy life free from addiction.

Get Started
Now
Call and speak with one of our caring team members about help for you or a loved one.






















